Understanding CBME
A paradigm Shift in Medical Education

The Competency-Based Medical Education (CBME) curriculum, introduced by NMC, marks a significant shift from a time-based, knowledge-centric approach to an outcome-based strategy. The core objective of CBME is to produce an “Indian Medical Graduate” (IMG) who is not only knowledgeable
but also possesses the necessary skills, attitudes, values, and responsiveness to function effectively as a physician of first contact in the community, while remaining globally relevant.
Key Principles of CBME:
Learner-Centric: The focus is on what the student should be able to do at the end of their training.
Patient-Centric: Training is geared towards providing preventive, promotive, curative, palliative, and holistic care with compassion.
Outcome-Oriented: Clearly defined competencies are the foundation, with teaching learning strategies and assessment methods designed to ensure these outcomes are achieved.
Integrated Learning: Emphasis on horizontal and vertical integration of subjects to break down traditional silos and foster a holistic understanding of medical problems, often using a problem-based learning approach.
Early Clinical Exposure: Providing students with early exposure to clinical settings to facilitate practical learning.
Skill Acquisition: A strong focus on developing practical skills, with certain essential skills requiring certification for independent performance.
Attitude, Ethics & Communication (AETCOM): Dedicated curriculum time for developing ethical values, responsiveness to patient needs, and effective
communication skills.
Formative and Internal Assessments: Streamlined assessment methods to align with the curriculum’s objectives
What is Flipped classroom technique?
The Flipped Classroom Revolution: Transforming General Surgery Education in the CBME Era
Introduction: Why Traditional Surgery Teaching Needs a Digital Makeover
Imagine walking into your general surgery rotation where instead of passive lectures about appendectomies, you’re actively practicing surgical decision-making through interactive case studies. Welcome to the flipped classroom model – a pedagogical revolution that’s reshaping medical education and perfectly aligning with Competency-Based Medical Education (CBME) principles.
In an era where medical knowledge doubles every 73 days, traditional “sit-and-get” lectures are becoming obsolete. The flipped classroom approach is emerging as a game-changer, particularly in general surgery education, where hands-on learning and critical thinking are paramount.
What is a Flipped Classroom in Medical Education?
Definition and Core Principles
The flipped classroom model inverts traditional teaching methods by:
- Pre-class Learning: Students engage with instructional content (videos, readings, simulations) before class
- Interactive Class Time: Face-to-face sessions focus on application, discussion, and skill practice
- Active Learning: Emphasis on problem-solving and collaborative learning
- Continuous Assessment: Real-time feedback and competency evaluation
Key Components for Surgery Education
Traditional Model | Flipped Classroom Model |
Lecture → Practice → Assessment | Pre-learning → Application → Immediate Feedback |
Passive listening | Active participation |
One-size-fits-all pace | Self-paced learning |
Limited interaction | Enhanced student-faculty engagement |
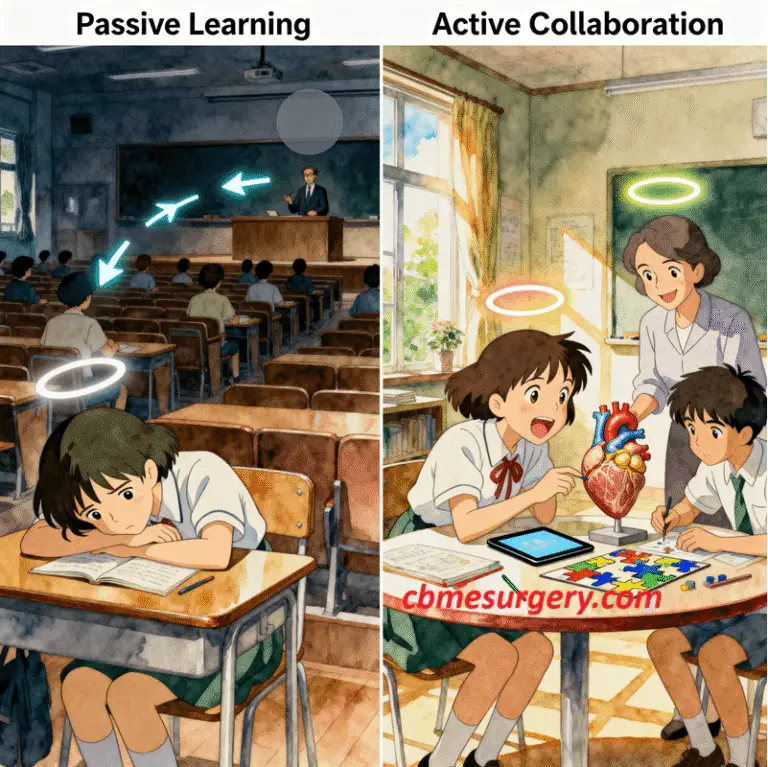
Comparison
Traditional classroom
(passive learning)
Vs
Flipped classroom
(active collaboration)
How Flipped Learning Enhances CBME Implementation
Competency-Based Medical Education focuses on outcomes rather than time spent learning. The flipped classroom model naturally supports this by:
- Milestone Achievement Tracking
- Real-time assessment during interactive sessions
- Immediate identification of competency gaps
- Personalized learning paths for each student
- Entrustable Professional Activities (EPAs) Integration
- Simulation-based practice during class time
- Progressive independence in surgical decision-making
- Mentor-guided skill development
- Continuous Feedback Loops
- Instant correction of misconceptions
- Peer-to-peer learning opportunities
- Faculty-student mentorship enhancement
Implementing Flipped Classrooms in General Surgery Training
Phase 1: Pre-Class Preparation (Home Learning)
Students engage with:
- Video Lectures
- Surgical anatomy demonstrations
- Operative technique breakdowns
- Case presentation reviews
- Interactive Modules
- Virtual reality surgical simulations
- 3D anatomical models
- Decision-making algorithms
- Reading Assignments
- Current literature reviews
- Clinical guidelines
- Evidence-based protocols
Phase 2: Classroom Application (Active Learning)
Interactive Learning Activities:
- Case-Based Discussions
- Complex surgical scenarios
- Multidisciplinary team simulations
- Ethical dilemma debates
- Skills Practice Sessions
- Suturing techniques
- Laparoscopic simulations
- Emergency procedure drills
- Problem-Solving Workshops
- Diagnostic challenges
- Treatment planning
- Complication management
Phase 3: Assessment and Feedback
Assessment Method | CBME Integration | Benefits |
Real-time quizzing | Milestone tracking | Immediate knowledge gaps identification |
Peer evaluation | Professional collaboration | Enhanced teamwork skills |
Simulation scoring | EPA progression | Objective skill measurement |
Reflective journals | Self-directed learning | Metacognitive development |
Benefits of Flipped Classrooms in Surgery Education
For Medical Students:
- Enhanced Learning Outcomes
- 23% improvement in knowledge retention
- Better critical thinking skills
- Increased engagement and motivation
- Flexible Learning
- Self-paced content consumption
- Repeated access to difficult concepts
- Accommodation of different learning styles
- Practical Skill Development
- More hands-on practice time
- Immediate feedback from instructors
- Peer learning opportunities
For Faculty Members:
- Efficient Teaching
- Reduced lecture preparation time
- More meaningful student interactions
- Better identification of struggling students
- Professional Development
- Technology integration skills
- Innovative teaching methods
- Research opportunities
Overcoming Implementation Challenges
Common Obstacles and Solutions:
- Technology Barriers
- Challenge: Limited access to digital platforms
- Solution: Institutional investment in learning management systems
- Tools: Blackboard, Moodle, Canvas integration
- Faculty Resistance
- Challenge: Comfort with traditional teaching methods
- Solution: Comprehensive training programs and gradual implementation
- Support: Peer mentorship and technical assistance
- Student Adaptation
- Challenge: Passive learning habits
- Solution: Clear expectations and scaffolded support
- Strategy: Gradual transition with increased accountability
- Content Development
- Challenge: Time-intensive resource creation
- Solution: Collaborative content sharing and institutional support
- Resources: Professional development funding
Global Trends and Future Directions
Current Adoption Rates:
- North America: 65% of medical schools implementing flipped models
- Europe: 45% adoption rate with rapid growth
- Asia-Pacific: 38% implementation with government support
- Developing Countries: 25% adoption with infrastructure challenges
Emerging Technologies:
- Artificial Intelligence Integration
- Personalized learning algorithms
- Intelligent tutoring systems
- Predictive analytics for student success
- Virtual and Augmented Reality
- Immersive surgical simulations
- 3D anatomical exploration
- Remote collaboration tools
- Mobile Learning Platforms
- Smartphone-optimized content
- Microlearning modules
- Offline accessibility
Conclusion: The Future is Flipped
The flipped classroom model represents more than just a teaching trend – it’s a fundamental shift toward competency-based medical education that prepares tomorrow’s surgeons for an increasingly complex healthcare landscape. By combining the flexibility of digital learning with the irreplaceable value of hands-on practice, we’re creating more engaged, competent, and confident medical professionals.
As medical education continues to evolve, institutions that embrace innovative teaching methods like the flipped classroom will lead the way in producing graduates who are not just knowledgeable, but truly capable of providing exceptional patient care.
Ready to Transform Your Surgery Education?
The journey toward flipped learning in general surgery education starts with a single step. Whether you’re a medical student seeking more engaging learning experiences or faculty considering pedagogical innovation, the flipped classroom model offers a pathway to enhanced competency-based education that benefits everyone involved.
