One-Minute Preceptor (OMP) in CBME: An Overview
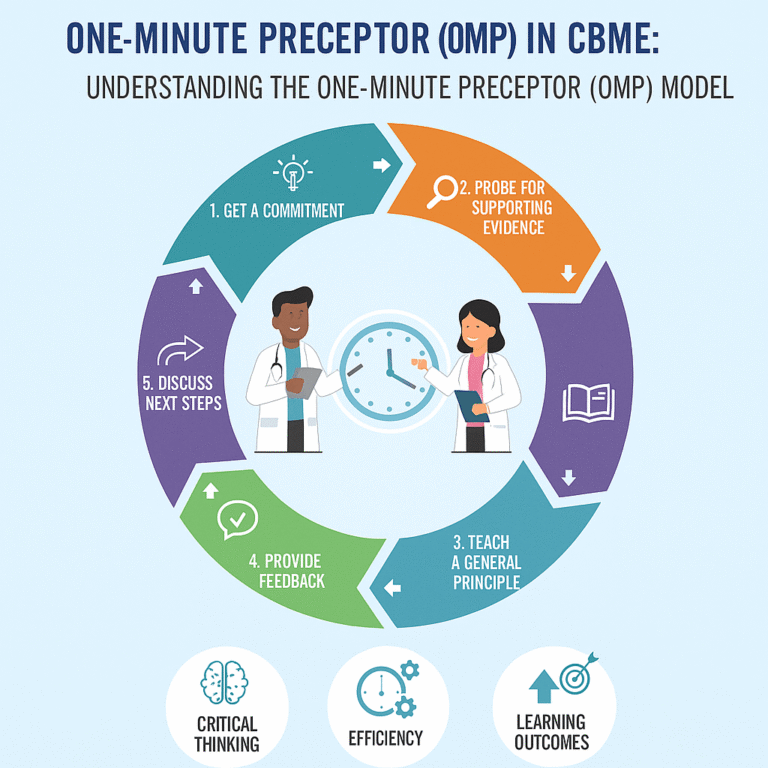
Understanding the One-Minute Preceptor (OMP) Model
The term “one minute” in the One-Minute Preceptor (OMP) model refers to the idea that effective teaching can be maximized within a brief timeframe—typically about one minute. The model is designed to fit into the fast-paced clinical environment, where educators may have limited time to engage with students. The focus is on concise, structured, and impactful teaching moments that can lead to significant learning outcomes in a short duration.
Detailed Breakdown of the One-Minute Preceptor (OMP) Model
The OMP framework consists of five key teaching steps, each designed to promote active learning, encourage critical thinking, and provide constructive feedback. Here’s a deeper exploration of each component:
- Get a Commitment
- Purpose: This step engages the student actively by prompting them to express their thoughts, ideas, or clinical reasoning regarding a specific case or scenario.
- Example: The teacher might ask, “What is your diagnosis for this patient?” This encourages the student to vocalize their assessment and fosters confidence.
- Probe for Supporting Evidence
- Purpose: This step encourages students to support their clinical decisions with evidence, promoting analytical thinking and reasoning.
- Example: The preceptor may ask, “What symptoms or test results influenced your diagnosis?” This prompts the student to think critically about their reasoning process and identify the basis of their clinical judgment.
- Teach a General Principle
- Purpose: To solidify learning, this step involves imparting a broader clinical principle or guideline relevant to the discussion.
- Example: After the student explains their reasoning, the preceptor might share a fundamental concept, such as, “Remember that in cases like this, consider the differential diagnoses based on age and presenting symptoms.”
- Provide Feedback
- Purpose: Timely, specific feedback is crucial for reinforcing learning and addressing any misconceptions the student may have.
- Example: The preceptor can respond with, “Your reasoning was solid, but remember to consider patient history more thoroughly in future evaluations.” This kind of feedback helps guide the student’s development.
- Discuss Next Steps
- Purpose: This final step focuses on guiding the student’s future learning pathway or clinical management based on the current case.
- Example: The preceptor might suggest, “I recommend you read about the management of this condition and then observe how we treat this patient in the next round.” This encourages continuous learning and application of knowledge.
Benefits of OMP in Clinical Education
- Efficiency: OMP maximizes the limited time available in busy clinical settings by creating structured and meaningful interactions that can be completed quickly.
- Active Learning: The model encourages student participation, fostering a more engaging learning environment.
- Critical Thinking: By probing the student’s rationale, the OMP instills a habit of thinking critically rather than just memorizing facts.
- Real-time Feedback: Immediate feedback helps students understand their strengths and areas for improvement, which enhances their learning and clinical skills over time.
- Reinforcement of Knowledge: Teaching general principles connects clinical scenarios to broader concepts, enhancing long-term retention of knowledge.
Conclusion
The One-Minute Preceptor model stands out as an effective teaching strategy within the framework of Competency-Based Medical Education. By leveraging brief, impactful interactions, this model cultivates essential skills in medical students, ultimately preparing them to be competent and thoughtful clinicians. Understanding and implementing the OMP approach can greatly enhance the educational experience for both learners and educators in the medical field.
Applying the One-Minute Preceptor (OMP) Model to a Case of a “Breast Lump Probably Malignant in a 50-Year-Old Female”
Here’s how you can use the One-Minute Preceptor (OMP) model to teach a medical student about managing a case involving a potentially malignant breast lump in a 50-year-old female patient.
Step 1: Get a Commitment
Question to the Student:
“What do you suspect the nature of this breast lump is, and what would be your initial approach for this 50-year-old female patient?”
Objective:
Encourage the student to articulate their preliminary diagnosis and management plan based on the clinical presentation.
Step 2: Probe for Supporting Evidence
Follow-up Question:
“Can you tell me what findings or risk factors led you to believe this lump might be malignant?”
Objective:
This encourages the student to consider contributing factors such as age, personal or family medical history, physical exam findings (like the size, consistency of the lump, lymph node involvement), and imaging studies (e.g., mammograms, ultrasounds).
Step 3: Teach a General Principle
Teaching Point:
“At this age, breast lumps have a higher risk of malignancy. It’s important to remember the significance of timing and follow-up; a fine-needle aspiration (FNA) or biopsy should be performed to obtain a definitive diagnosis.”
Objective:
Emphasize the importance of age as a risk factor for breast cancer and the need for diagnostic procedures when a lump is suspicious. This links the specific case to broader principles of breast cancer evaluation.
Step 4: Provide Feedback
Feedback Response:
“Your approach to suspecting malignancy is good given her age and the characteristics of the lump. Just ensure you also consider a thorough history and physical examination. What would you ask or note specifically?”
Objective:
Point out what the student did well and where they might need to refine their approach, enhancing their clinical reasoning and history-taking skills.
Step 5: Discuss Next Steps
Next Steps Guidance:
“I’d recommend that you review the guidelines for breast cancer screening and management. Make sure to discuss with the patient the need for imaging and possible biopsy options. Also, think about referral to a specialist, such as a surgeon or oncologist, depending on the results.”
Objective:
Encourage the student to take ownership of the ongoing care plan, emphasizing the importance of follow-up, patient education, and multidisciplinary collaboration.
Conclusion
By using the One-Minute Preceptor model in the context of a potentially malignant breast lump in a 50-year-old female, educators can effectively engage students in critical thinking while providing them with the tools to navigate similar clinical scenarios in the future. This structured approach not only enhances learning but also prepares future clinicians to manage patient care with confidence and competence.
